Special
check-ups
Accueil » Bilans Spéciaux
Practical services, designed to fit into your daily life
Because some questions cannot always be answered by conventional analyses, this section gives you access to a selection of check-ups designed to refine prevention, clarify a doubt or guide you toward more personalized treatment.
Targeted check-ups, to better understand before taking action
Certain situations require going beyond standard analyses.
Special check-ups that are proposed can help refine prevention measures, explore a disorder or guide lifestyle changes.
Whether your are a doctor or therapist, our team will support you with the implementation of targeted analyses, adapted to your practise.
If you use connected prescriptions, you can directly create your own check-ups.
If necessary, we can prepare them for you, according to your desired parameters.
- Do you want to talk more about it? You can contact our main office at +41 22 309 15 20
(Monday to Friday: 7:30 a.m. – 6:30 p.m.) - For non-urgent requests, please contact us at info@labomgd.ch
Fax: 022 343 30 44
Our team will put you in touch with a specialist or medical representative.
Fatty acids
Erythrocyte fatty acids and phospholipid-bound fatty acids
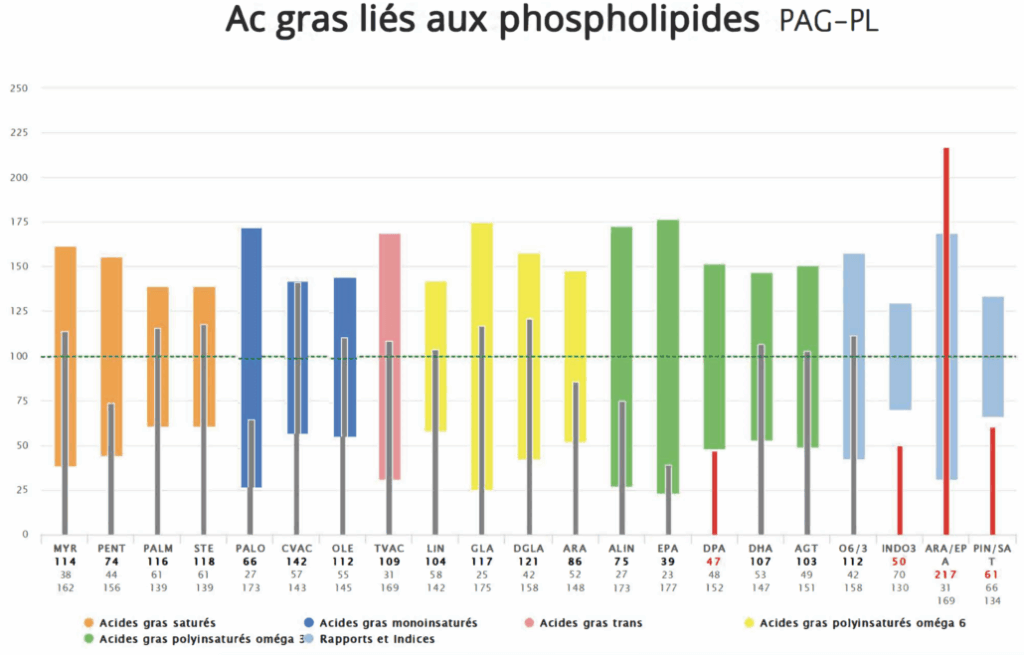
It is possible to request a fatty acid analysis, either for those present in erythrocyte membranes (erythrocyte fatty acids) EFAP, or those bound to phospholipids present in the bloodstream PLFA.
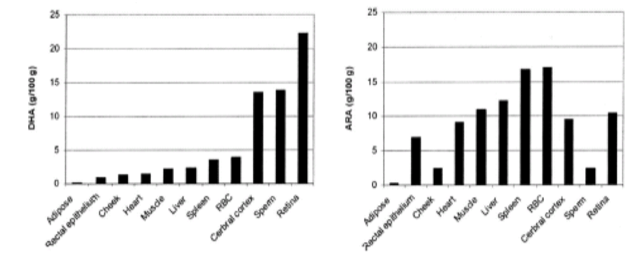
- Cells in each tissue have a membrane with its own unique FA composition, with different preferences and ratios: concentrations are not the same in erythrocytes as in retinal or brain cells, for example.
However, erythrocyte membranes have polyunsaturated fatty acid concentrations roughly equivalent to those found in the cardiac muscle and are therefore a useful tool for cardiovascular prevention. This profile is the most used one. - Fatty acids linked to phospholipids represent what is available to the entire body (brain, heart, skin, perisplanchnic fat).
In practise, both profiles are similar, in particular for normal profiles.
It is important to always request the same profile for medical follow-up.
Erythrocyte fatty acids reflect the diet of the last 3 to 4 months, due to the lifespan of erythrocytes, while PLFA represent changes over the last 6 to 8 weeks.
Therefore, both profiles are suitable for medium and long-term estimations of the nutritional check-up, which is quite independent of sporadic dietary excesses (e.g., meals from the previous day or week prior to testing).
Chart
Concentrations of omega-3 DHA and omega-6 ARA (arachidonic acid) in different organs and in erythrocytes (RBC Red Blood Cells).
The fatty acid (FA) check-up completes the cholesterol check-up by identifying risk factors for inflammatory and cardiovascular diseases.
→ For a scientific text with bibliography, see the following link: AGE_final_June 29th, 2021
Fatty acids have various effects on cardiovascular metabolism, including:
- Saturated fatty acids (no double bond): may increase LDL and decrease HDL. They can worsen cardiovascular risks.
- Omega 6 polyunsaturated fatty acids: they are useful for immunity yet can be inflammatory when in excess.
- Omega 3 polyunsaturated fatty acids: they favor membrane plasticity and can be anti-inflammatory and protective against atherothrombosis.
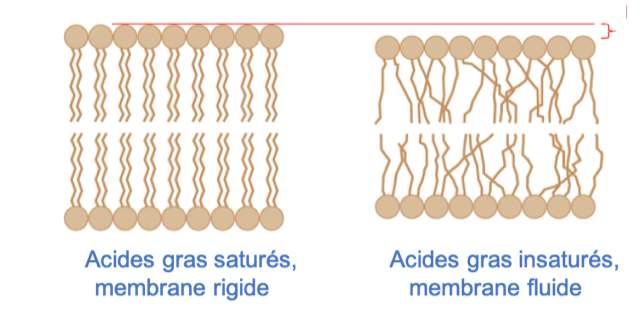
Example of membrane structures:
By stiffening membranes, saturated fatty acids limit transmembrane transport and intercellular contact, among other things. On the contrary, polyunsaturated fatty acids, through double bonds that reduce membrane thickness and free up space between fatty acid chains, promote much more active transmembrane circulation.
Erythrocyte fatty acids and phospholipid-bound fatty acids
It is possible to request a fatty acid analysis, either for those present in erythrocyte membranes (erythrocyte fatty acids) EFAP, or those bound to phospholipids present in the bloodstream PLFA.
- Cells in each tissue have a membrane with its own unique FA composition, with different preferences and ratios: concentrations are not the same in erythrocytes as in retinal or brain cells, for example.
However, erythrocyte membranes have polyunsaturated fatty acid concentrations roughly equivalent to those found in the cardiac muscle and are therefore a useful tool for cardiovascular prevention. This profile is the most used one. - Fatty acids linked to phospholipids represent what is available to the entire body (brain, heart, skin, perisplanchnic fat).
In practise, both profiles are similar, in particular for normal profiles.
It is important to always request the same profile for medical follow-up.
Erythrocyte fatty acids reflect the diet of the last 3 to 4 months, due to the lifespan of erythrocytes, while PLFA represent changes over the last 6 to 8 weeks.
Therefore, both profiles are suitable for medium and long-term estimations of the nutritional check-up, which is quite independent of sporadic dietary excesses (e.g., meals from the previous day or week prior to testing).
Chart
Concentrations of omega-3 DHA and omega-6 ARA (arachidonic acid) in different organs and in erythrocytes (RBC Red Blood Cells).
Oxidative stress check-up
To be completed with explanations on hydrophilic antioxidants and nadh and gpx regeneration.
For reasons of simplicity and in order to spread the costs of certain dosages which are not necessarily covered by health insurance companies, we offer several check-ups.
CAROTENOIDS
This check-up evaluates concentrations of lipophilic antioxidant molecules (β-Carotene, lutein, etc.).
ANTIOXIDANTS
This group includes two screening tests for oxidative stress activity and defenses, namely FORD and FORT. These include two ubiquitous antioxidants, Coenzyme Q10 (CoQ10) and uric acid. Reduced glutathione gives an indication of the antioxidant enzame activity. Oxidized anti-LDL antibodies give an indication of immune defenses against oxidized LDL, especially active in atherosclerosis and stroke (among other things).
In the urine, 8-hydroxy-2′-deoxyguanosine dosage (8-OH-DG) is very interesting as it gives information on the quantity of daily mutations with which the cells of the body are confronted. These sporadic mutations, directly dependent on oxidative stress (free radicals), are normally eliminated by various cellular systems (apoptosis, etc.). When they are in excess and the antioxidant defenses are minimal, these DNA mutations may persist and reproduce, opening the door to tumor proliferation.
SMALL OXIDATIVE STRESS CHECK-UP
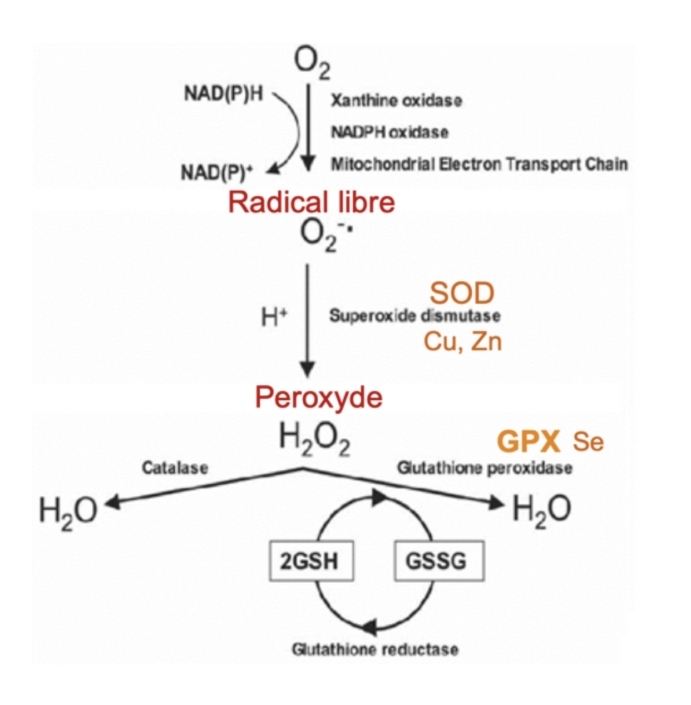
By complementing the FORD and FORT tests for oxidative stress activity and defenses, this check-up evaluates the enzymatic activity responsible for eliminating free radicals, namely SOD and GPX, and the cofactors required for this activity, which are copper, selenium and zinc.
MAJOR OXIDATIVE STRESS CHECK-UP
In addition to the analyses of the small oxidative stress check-up and the others described above, this check-up evaluates two vitamins: one antioxidant, vitamin E, and the other, vitamin A, which is not strictly speaking an antioxidant, but is found at the end of carotenoid metabolism, and as such, is an indirect marker of lipophilic antioxidants. Transferrin and ferritin offer insight into liver inflammatory processes and iron metabolism, which is important in the cardiovascular protection processes.
Physiology and biology of oxidative stress
To understand these dosages, it may be useful to review the physiology and biochemistry of oxidization mechanisms.
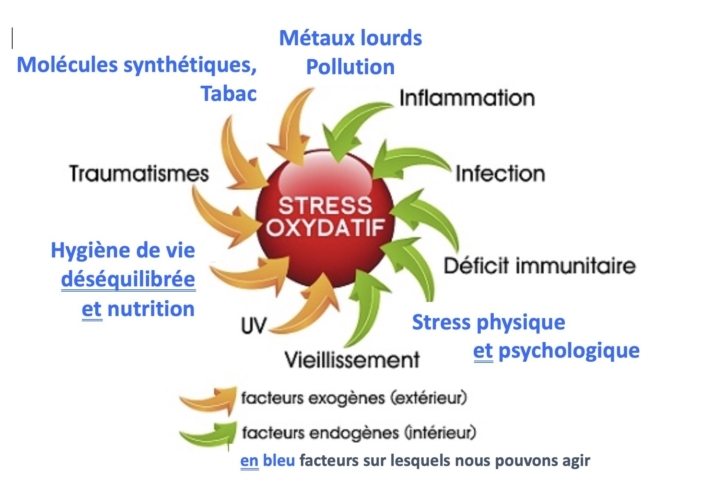
It is estimated that 50-70% of diseases are directly or indirectly linked to a poor management of oxidative stress.
Antioxidants
Lipophilic antioxidants include carotenoids and CoQ10. Hydrophilic antioxidants are represented by uric acid antioxydants.
Coenzyme Q10, also known as Coenzyme Q, CoQ or ubiquinone, is a 1.4-benzoquinone for which “Q” refers to the quinone group and “10” to the number of isoprenic units in its side chain.
This substance, similar to a a fat-soluble vitamin, is found in almost every eukaryote cell, mostly in mitochondria, where it participates in the respiratory chain, as part of aerobic cellular respiration.
In every cell, including red blood cells, there are different mechanisms for transforming complex molecules, which are not degraded by traditional enzymatic pathways, into easily eliminated metabolites, including drugs and environmental toxins.
Therefore, there are mechanisms that use the oxidative action of oxygen, chlorine, nitrogen, to produce free radicals (Reactive Oxidative Species or ROS).
The oxygen pathway involves at least two enzymes: SOD – superoxide dismutase – and GPX – glutathione peroxidase. Free radicals, which are highly toxic but also highly effective, are metabolized into peroxides by SOD with the cofactors copper and zinc, and then converted into water by the GPX/glutathione system. GPX uses selenium as cofactor. Other pathways, such as the catalase one, complete these purification mechanisms.
A deficiency in cofactors or a SOD/GPX imbalance, causes poorly managed oxidative stress, whose consequences can lead to cardiovascular disease, diabetes, hepatitis and cancer.
Vascular and cardiometabolic risk check-ups
Cardiometabolic risks I
This check-up mainly targets lipid metabolism, with a HOMA and ferritin approach to metabolic syndrome.
Dosages: HS-CRP, Lp(a), ApoA1/B, Apo-CIII, glycerol, anti-oxidized LDL, ferritin, HOMA, Quicki, IGF-1.
Find out more:
HS-CRP (High-sensitivity CRP): marker of micro-inflammation between 1 and 5. If more, it may be a sign of an important stress.
Lipoprotein (a): independent marker of cardiovascular risks.
Apo B/Apo A1: high Apo B accelerates transport of LDL to targeted organs.
This is an additional and independent risk of LDL level.
Apo-CIII: linked to the synthesis of triglycerids, may increase before triglycerids. It is an early marker of CV risks in normolipid subjects and a predictive factor of coronary lesion progression.
Glycerol: the best marker of free fatty acid (FFA) concentrations.
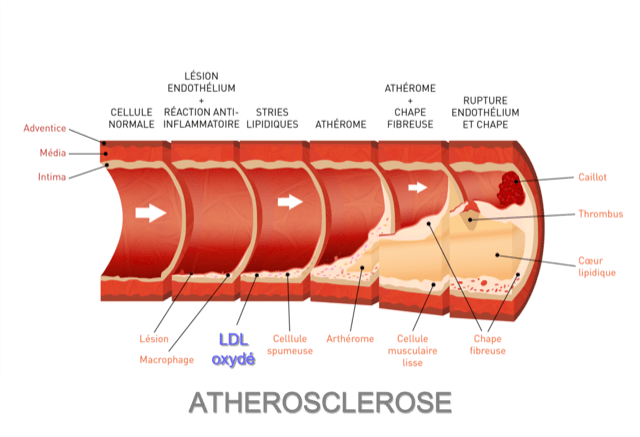
Anti-oxidized LDL and oxidized LDL: LDL, in the presence of free radicals (oxidative stress) is oxidized and promotes the formation of unstable frothy atheromatous plaques, which can be released and cause a stroke. Direct concentrations of oxidized LDL are offered in addition, to which is added the dosage of anti-oxidized LDL antibodies, which may play a protective role against oxidized LDL.
Ferritin: elevated ferritin may be secondary to iron overload or liver inflammation. Ferritin can result from iron deficiency: 30 to 50% of heart failure patients are iron deficient.
HOMA and Quicki: a high HOMA index or a low Quicki suggest a resistance of peripheral tissues to insulin. In the long-term, this condition is likely to favor the development of type 2 diabetes.
IGF-1: IGF-1 dosage for insulin resistance and cardiovascular risk is useful in high-protein and high-calorie eaters. Some athletes fall into this group, as do those taking “vitamin and protein” supplements.
Cardio-metabolic risk II
This check-up is more complete and takes into account other predictive factors linked to nutrition (IGF-1), iron metabolism (hepcidin) and endotoxins. It introduces oxidative processes as aggravating situations.
Dosages: HS-CRP, Lp(a), Apo A1/B, Apo-CIII, glycerol, anti-oxidized LDL, ferritin, HOMA, Quicki, hepcidin, IGF-1, LBP, thioredoxin, glutathione, TMAO.
Find out more:
- Hepcidin: hepcidin participates to iron homeostasis. High expression of hepcidin causes iron to accumulate in cells; low expression causes iron to be released into the extracellular environment. Its dosage enables to better understand the causes of iron deficiency. Iron deficiency may explain chronic fatigue and is also a cardiovascular risk factor.
- LBP: molecules include endotoxins, toxins present on the surface of Gram (-) bacteria. They induce an immune response at a distance from the site of infection.
- Thioredoxin: thioredoxin (TRX1) is an enzyme acting as antioxidant by making the reduction of other proteins easier. It plays an anti-inflammatory, antioxidant and anti-apoptotic role. It is found in almost every cell.
- Glutathione: glutathione is also involved in a number of detoxification and reactive oxygen species elimination reactions. Glutathione is vital for detoxifying heavy metals such as mercury, lead and cadmium, and many other pollutants. Glutathione reacts with the salts of these heavy metals, creating a very strong bond so that they can be excreted without causing any damage to the body, apart from loss of glutathione and slight acidification.
- TMAO: TMAO is produced by certain intestinal bacteria. Levels of TMAO in blood are associated with heart diseases. There is a link between TMAO levels and the risk of future serious cardiovascular events, even in patients with no prior indication of cardiac risk.
Cardiovascular risk
This third check-up is targeted differently from the first one, taking into account an aggravating factor, homocysteine, and a ubiquitous antioxidant, Co-enzymeQ10.
Dosages: Fatty acids, Lp(a), Apo A1, Apo B, HOMA, anti-oxidized LDL, homocysteine, coenzyme Q10.
Find out more:
Fatty acids: The fatty acid check-up complements the cholesterol check-up by identifying risk factors for cardiovascular and inflammatory diseases.
Fatty acids have various effects on cardiovascular metabolism, such as:
- Saturated fatty acids (no double bond): They may increase LDL and decrease HDL; they can worsen cardiovascular risks.
- Polyunsaturated fatty acids Omega 6: They are both useful for immunity but inflammatory in excess.
- Polyunsaturated fatty acids Omega 3: They favor membrane plasticity and they can be anti-inflammatory or protective against atherothombosis
- Homocysteine: Homocysteine favors cardiovascular disorders due to its adverse effects on cardiovascular endothelium and smooth muscles cells.
- Coenzyme Q10: CoQ10 is found in every human cell and plays a role in transforming energy from food into energy that can be used by the cell. It is a great antioxidant, complementing the antioxidant effect of lipophilic molecules such as carotenoids.
Antioxidant carotenoids
Note: Carotenoids are part of a family of molecules whose functions include neutralizing oxidative stress. Other molecules, such as vitamins C and E, and Coenzyme Q10, play complementary roles. Carotenoids are lipophilic, which means they are more easily absorbed when oils are added to foods, such as carrots in salads rather than ate as they are.
- Lutein and zeaxanthin: they are found in lens, which act as antioxidant and protect against UV rays. They help prevent macular degeneration.
- β-Cryptoxanthin: a light antioxidant that complements the role of other carotenes. It serves as an indicator of dietary diversity. It is also thought to protect against certain cancers.
- Lycopene: a particularly good antioxidant that can play a role in protecting the skin against UV rays, prostate, and against atherothrombosis. It is found in tomatoes, especially sun-dried tomatoes and tomato “ketchup”.
- α-Carotene and β-Carotene: good antioxidants (especially beta), precursors of vitamin A. May play an anti-cancer role.
Note: There are specific disease markers, such as breast cancer markers which require genetic advice. The markers presented here are designed to evaluate risks, not specific cancers.
MTHFR
The protein-coding gene for MTHFR detects a DNA sequence associated with increased blood homocysteine concentrations. This may increase the risk of premature cardiovascular disease, thrombosis and stroke. Around 10% of the French population is homozygous for C677T.
CARDIOgen
This test analyzes polymorphisms involved in oxidative stress, homocysteine and lipid metabolism disorders, high blood pressure and thrombosis formation.
CARDIOgen is recommended in case of family history of cardiovascular diseases, suspicion of cardiovascular diseases, homocysteine or lipid metabolism disorders and high blood pressure.
LIPIDgen
LIPIDgen analyzes genetic polymorphism involved in atherosclerosis development and its underlying causes such as lipid metabolism disorders.
LIPIDgen is recommended for people with a history of type III familial hypercholesterolemia or atherosclerosis, or for those with high level of HDL, LDL or total cholesterol.
THROMBOgen
THROMBOgen analyzes polymorphisms involved in hemostasis, formation of blood clots and folate metabolism. The information obtained enables measures to be taken to reduce the relative risk of thrombosis. THROMBOgen is indicated in case of family history of thrombosis, before taking oral contraception, in case of recurrent spontaneous abortions and atherosclerosis in young people.
METHYLgen/OPTIMETgen
Methylation is one of the essential biochemical processes that occur continuously in all cells. For example, it is involved in the running of protein expression, heavy metal and neurotransmitter modification, and xenobiotic detoxification.
Genetic markers
Contact: service-melisa@labomgd.ch
Melisa is a Lymphocyte Transformation Test (LTT), during which memory lymphocytes are cultured during 5 to 6 days in the presence of the suspected allergen.
This test differs from a traditional proliferation test because it involves culturing 106 cells (instead of the 105 cells usually used), depleting adherent cells (macrophages), and using inactivated human serum instead of fetal calf serum in order to increase sensitivity by reducing spontaneous proliferation.
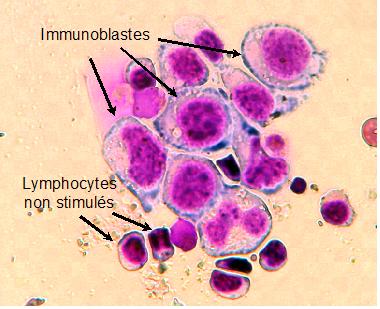
Proliferation is measured by the incorporation of radioactively labeled thymidine (3H-thymidine) by stimulated memory cells which diversify and differ from lymphoblasts. The proliferation of cells cultured in the presence of allergens is compared to that of cells cultured without allergens and expressed as a stimulation index (SI).
A SI between 2 and 3 is interpreted as “possible sensitization”, a SI ≤ 2 is considered as negative.
Cells cultured for 5 days are also morphologically analyzed after cytocentrifugation and staining (Figure 1).
Only tests with positive radioactivity counts and morphology showing lymphoblasts are considered positive.
This technique is a modern immunotoxicological method for detecting sensitivity to metals, infectious agents, and metabolites from food and drugs.
Download the prescription sheet:
Application and conditions for analysis:
The MELISA® test as a diagnostic tool for metal allergies
Metal exposure source
- Amalgams, dental implants
- Prosthesis
- Jewellery
- Food
- Medicine
- Cosmetics
- Vaccines
- Pollution
- Tobacco
- Prenatal exposure
In dentistry, titanium dioxide (TiO2) is used as a white pigment and for its bactericide properties. In the food and pharmaceutical industry, it is used as colorant.
Titanium (Ti) is often used in surgery (prosthesis).
Cadmium (Cd), palladium (Pd) and lead (Pb) are found in dental colorant preparations.
Mercury (Hg) makes up to 50% of the composition of dental amalgams.
Nickel (Ni), zinc (Zn), indium (In), gold (Au), copper (Cu) and platinum (Pt) are present in the form of alloys, crowns, and dental prostheses.
Mercury derivatives (thimerosal, ethylmercury, phenylmercury) are used in dentistry as preservatives.
Thimerosal is used as preserving agent in nasal and ocular solutions as well as in certain immunoglobulin-based vaccines.
Silver (Ag), gold (Au), nickel (Ni), copper (Cu) and tinplate are often used in jewellery.
Tinplate is also found in utensils and food containers.
Immunological definition of a metal allergy
Several metals widely used in medical and dental care (particularly nickel, gold, palladium and mercury) can sensitize genetically predisposed individuals and induce a type IV allergic reaction.
In contrast to type I allergy triggered by IgE immunoglobulin, the type IV allergy is mediated by T lymphocytes that have previously been in contact with allergens, hence their name “memory lymphocytes”.
Following re-exposure to a sensitizing allergen, memory lymphocytes will respond with morphological transformation (lymphoblastic transformation) and their proliferation through cell division will be initiated.
The cells produced and stimulated in this way will initiate an allergic reaction through cytokines.
Symptoms observed following a metal allergy
A chronic metal exposure may be the cause of several symptoms such as allergy, Chronic Fatigue Syndrome (CFS), multiple sclerosis, fibromyalgia and Multiple Chemical Sensitivity (MCS).
Allergenic metals
The most common are: nickel, cadmium, gold, beryllium, titanium, palladium, indium, lead, mercury, tinplate, platinum, chromium and cobalt.
The industries most affected by metal poisoning
Building (bricklayers) and mining sectors: chromium and cobalt.
Electricians and photographers: chromium.
Aerospace manufacturers: beryllium.
Hair salon and cosmetic product users: nickel, titanium.
Metal industry: nickel, chromium, cobalt and mercury.
Paper, wood and leather industries: chromium.
Painters: chromium, cobalt.
Textile industry, dentists and dental technicians: nickel, mercury.
Allergenic metals are present in everyday products
Jewellery, dental implants, cosmetics, prostheses, stents, coins…
Metal sensitivity test
Metal sensitivity is usually diagnosed by a “patch-test”. Although a positive reaction may indicate a specific allergy to an antigen, the “patch-test” has many disadvantages, including the difficulty of distinguishing an allergic reaction from a nonspecific irritant reaction, low sensitivity and reproducibility, and a risk of sensitization.
Moreover, this method is only significant for allergens whose main route of sensitization is cutaneous.
The MELISA test offers another diagnostic alternative that has been medically validated and does not have the disadvantages observed in the conventional patch test method. Furthermore, reproducibility, sensitivity, specificity, and reliability tests have confirmed the value of the test as a diagnostic tool (Valentine-Thon and Schiwara, 2003).
Consequence of metal poisoning
Metals bind to sulfur groups (SH) in cells and enzymes of the body.
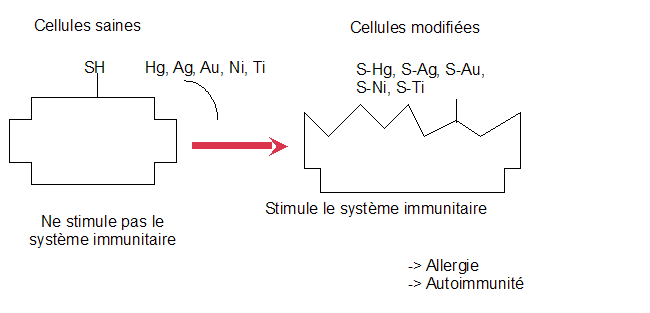
Furthermore, metals (Pb, Cd, Hg, and As in particular) could also induce oxidative stress, interfering with lipid and protein synthesis or carcinogenesis through the oxidation of nucleic acids.
Some bibliographical references
- Sicilia A., Cuesta S., Coma G., Arregui I., Guisasola C., Ruiz E., Maestro A. (2008). Titanium allergy in dental implant patients: a clinical study on 1500 consecutive patients. Clin. Oral Impl. Res. 19: 823-835.
- Stejskal V.D.M., Hudecek R., Stejskal J., Sterzl I. (2006). Diagnosis and treatment of metal-induced side-effects. Neuroendocrin. Lett. 27 (Suppl 1): 7-16.
- Stejskal V.D.M., Danersund A., Lindvall A., Hudecek R., Nordman V., Yaqob A., Mayer W., Bieger W., Lindth U. (1999). Metal-specific lymphocytes: biomarkers of sensitivity in man. Neuroendocrin. Lett. 20: 57-64.
- Stejskal V.D.M. (1997). Human hapten-specific lymphocytes: biomarkers of allergy in man. Drug Information Journal. 31: 1379-1382.
- Stejskal V.D.M., Cederbrant K., Lindvall A., Forsbeck M. (1994). Melisa – an in vitro tool for the study of metal allergy.Toxic. in vitro. 5: 991-1000.
- Stejskal V.D.M., Olin R., Forsbeck M. (1986). The lymphocyte transformation test for diagnosis of drug-induced occupational allergy. Journal of allergy and clinical immunology. 77: 411-426.
- Valentine-Thon E. and Schiwara H-W. (2003). Validity of MELISA for metal sensitivity testing. Neuroendocrin. Lett. 24: 289-298.
MELISA MEDICA FOUNDATION: website (where most of the reference articles can be downloaded)
Melisa
Lipid metabolism includes the usual cholesterol check-up with the addition of additional markers that may play a role in aggravating cardiovascular disease, among other conditions.
- Homocysteine: it favors cardiovascular disorders due to its adverse effects on endothelium and smooth muscles cells.
Journal: Gangulyand Alam Nutrition Journal 2015, 14:6 - Apo B vs Apo A1: high Apo B accelerates the transport of LDL to targeted organs. This is a cumulative and independent risk factor that adds to the LDL level.
- Lipoprotein (a): independent marker of cardiovascular risks.
Journal: Lipoprotein(a) : a historical appraisal. Journal of LipidResearch, 1–14. doi:10.1194/jlr.r071571 - Oxidized LDL: LDL, in the presence of free radicals (oxidative stress), is oxidized and favors the formation of unstable frothy atherosclerotic plaques in the arteries, which can be released and potentially cause a stroke. Direct concentrations of oxidized LDL are measured, to which is added the measurement of anti-oxidized LDL antibodies, which may play a protective role against oxidized LDL.
Journal: LDL oxydé : Can J Cardiol. 2017 Dec;33(12):1624-1632. doi: 10.1016/j.cjca.2017.07.015. Epub2017 Jul29 , Anticorps LDL oxydé : Curr Pharm Des. 2007;13(10):1021-30.
Métabolisme des lipides
Neurotransmitters-1
The neurotransmitter check-up covers the following neurotransmitters:
Adrenaline, Norepinephrine and their metabolites, MHPG and VMA
Dopamine, its precursor DOPA and its metabolite HVA
Serotonin, its precursor Tryptophane and its metabolite 5-HIAA
BDNF « Brain Derived Neurotrophic Factor »
GABA and Glutamate
Link to the full text: Neuro_08_2021
Lymphocyte profile
This profile explores immune processes in their entirety, excluding recognized severe pathologies and organ transplantation. It is useful for prevention and to evaluate immunity. The participation and role of the different markers is presented in the following check-ups.
CD3, CD4, CD8, B, NK, CD57
Without being as complete as the Lymphocyte profile, this profile provides a check-up of the immune status of the patient. It reveals the immune defense state during and after an infectious episode.
Th17, Th22, CD25
This profile evaluates helper lymphocytes, which have a protective immune function and contribute to the implementation of an immune response during bacterial and fungal infections. CD25+ regulatory lymphocytes are the expression of an immune tolerance: they suppress the specific IgE synthesis.
Th1, Th2
The participation of Th1 and Th2 helper lymphocytes alone explains most of the immune responses that occur in infectious and inflammatory diseases. Autoimmune diseases are associated with an uncontrolled and excessive type Th1 response by the immune system. Th2 isinvolved in immediate hypersensitivity reactions with the production of antigen-specific IgE and allergic responses. The protective immune response is Th1-type during an infection caused by intracellular pathogens and Th2-type when extracellular organisms are involved (anti-parasite action).
General introduction
In the body, two immune systems overlap:
- Natural immunity (innate): quick, nonspecific, directed against anything foreign to the body. These include: natural defense barriers (skin, mucous membranes), various secreted substances (cytokine proteins).
Monocytes, granulocytes, NK cells. - Acquired immunity: slow, but specific to a component, make the distinction between self and non-self. It is adaptive: it strengthens after a new contact (=anamnestic reaction). The cells involved are B cells [= humoral immunity (Ig)], and T cells [= cellular immunity (cytokines; direct action)].
- B lymphocytes: responsible for acquired immunity and produce immunoglobulin antibodies. Their antibodies bind directly to an antigen for which they are specific.
- T lymphocytes: T lymphocytes play a role in the secondary immune response. “T” is the abbrevation for thymus, where their development ends.
Responsible for cellular immunity: the cells infected by a virus, or the cancerous cells recognized as foreign (which means distinct from the cells that T lymphocytes have learned to tolerate during their maturation) are destroyed. They are used in patients with AIDS, with CD3, CD4 and CD8, referring to characteristic antigens on the surface of different subtypes of T lymphocytes. - NK lymphocytes: NK lymphocytes (Natural Killer) are cells of the innate immunity. These are large granular lymphocytes, non-T (CD3-) and non-B (CD19-), characterized in humans by the markers CD56, CD16, and NK.
Detailed description of different profiles
Immunophenotyping, cellular immune status and control parameters
A lymphocyte profile (also known as immunophenotyping) evaluates the immune status and highlights potential pathology situations. It also monitors T lymphocytes levels at the end of an organ transplantation.
Immunophenotyping is recommended in case of cellular immune deficiency and immunodeficiency with recurrent or chronic infections. Most antigens detected by immunophenotyping are identified by a CD (Cluster of Differentiation) followed by a number.
Lymphocyte profile CD3, CD4, CD8, B, NK, CD57
CD3+ T cells
As the other hematopoietic cells, T lymphocytes come from a totipotent stem cell, present in bone marrow. CD3 is the common antigen used to identify T lymphocytes. In peripheral blood, T lymphocytes are characterized by the expression of a membrane marker called CD3 and a specific receptor called TCR (T cell receptor), which is directly involved in antigen recognition.
CD4+ T helper cells have non-cytotoxic activity and act as intermediaries in the immune response. CD4+ T cells play an essential role in inducing and regulating immune responses. These lymphocytes proliferate only when bound to pathogenic antigens to activate other types of cells that will act more directly on the response, hence their name as helper cells. CD4+ T lymphocytes excrete interleukin-2 (IL-2), a cytokine which act as a chemical intermediary between T and B lymphocytes, by stimulating their proliferation. Once bound to the antigen, naive CD4+ T cells proliferate and differentiate into activated helper cells or “memory” cells.
CD8+ T helper cells are responsible for eliminating infected cells. CD8+ T cells recognize and attack only specific antigen-presenting cells presented by antigen-presenting cells (APCs) such as B cells, dendritic cells, and macrophages.
The CD4+/CD8+ ratio is considered as a marker of immune restoration from residual activation and inflammation. To this day, there is no clear mechanism explaining the expansion of this population and their pathogenic role, although the existence of an immune deficiency appears to play a major role.
B lymphocytes
B lymphocytes form and mature in the bone marrow. After maturation, B lymphocytes gather in the lymph nodes, spleen, and other lymphoid tissues where they can come into contact with the antigens for which they are specific. B lymphocytes can act as antigen-presenting cells (APCs). These lymphocytes are the main cells involved in the adaptive immune response through the production of antigen-specific antibodies.
Natural Killer (NK) cells are part of the body’s first line of defense. NK cells account for 5 to 16% of lymphocytes and belong to the innate immune system due to their invariant receptors. These non-T (CD3-) and non-B (CD19-) lymphocytes are capable of lysing cells foreign to the body independently of antigen and without prior activation, unlike CD8+ T cells. There are two types of NK cells, divided according to the density of CD16 and CD56 membrane marker expression.
CD8+/CD57+ T cells are activated cytotoxic T lymphocytes whose development follows chronic antigenic stimulation. A polyclonale growth of CD8+/CD57+ T cells may be observed in different pathological situations, such as chronic viral infection or immune deficiency. This population of lymphocytes results from chronic stimulation of CD8+/CD28+ cells by exogenous antigens of infectious origin, leading to the generation of CD8+ cells that gradually lose their ability to proliferate due to the loss of CD28 antigen expression. Meanwhile, on their surface, they express the CD57 antigen. CD8+/CD57+ T cells represent 1 to 15% of total lymphocytes in healthy subject. Their number and proportion progressively increase with age. This lymphocyte population increase particularly during disease such as HIV infections or transplant rejections reactions. CD8+/CD57+ T cells release cytolytic and cytotoxic substances, capable of inhibiting polyclonal activation and immunoglobulin production. The analysis of CD57+ cells enables therapeutic follow-up during and after Lyme disease diagnosis.
Lymphocyte profile Th17, TH22, CD25
CD4+ Th17 T cells represent a third class of T helper lymphocytes, the first two being CD4+ Th1 et Th2 T cells.
The three CD4+ helper cell populations Th1, Th2, and Th17, are distinguished by their cytokine profile and the type of chemokine receptors expressed on their surface. CD4+ Th17 T cells have a protective immune function that contributes to the establishment of an immune response during fungal and bacterial infections. Activation of the Th17 population pathway seems to be linked to inflammatory and autoimmune diseases, such as psoriasis, rheumatoid arthritis, certain forms of asthma, multiple sclerosis and chronic bowel diseases. The characteristic feature of Th17 cells is the production of IL-22. IL-22 acts on non-hematopoietic cells such as epithelial cells in the digestive or pulmonary systems. In the epidermis, IL-22 acts on epidermal keratinocytes and participates in epithelial homeostasis.
Th22 T helper cells are distinct from regulatory T cells that express the surface marker CD25. This differentiation of CD4+ T lymphocytes reflects adaptive immune defense. The balance between these various lymphocyte subpopulations is essential to the immune homeostasis and host defense. Its breakdown contributes significantly to the onset of inflammatory autoimmune diseases, chronic infections, allergies, and asthma. The evolution of CD4+ Th17 and Th22 T lymphocyte populations are markers of chronic inflammation. The incidence of chronic inflammatory diseases and inappropriate immune responses is significantly higher in people with an altered microbiota (dysbiosis), due to diet and sedentary lifestyles, than in those with healthy microbiota. Dysbiosis creates a favorable environment for infections caused by pathogens and the development of chronic conditions.
Antigen-specific CD4+ CD25+ regulatory T cells are an expression of immune tolerance. CD4+ CD25+ T cells suppress specific IgE synthesis.
Lymphocyte profile Th1, Th2
CD4+ T lymphocyte populations are distinguished based on their functional abilities to produce different cytokine profiles.
The participation of CD4+ Th1 and CD4+ Th2 helper T cells alone explains most of the immune responses that occur in infectious and inflammatory diseases. Autoimmune diseases are associated with an uncontrolled and excessive Th1 response by the immune system.
CD4+ Th1 T cells mostly produce IL-2, TNF and IFNget, and are involved in cellular immune responses (reactions of late hypersensitivity, activation of macrophages and cytotoxic activity). CD4+ Th2 T cells excrete IL-4, IL-5, IL-6 and IL-13 cytokins. They are involved in immediate hypersensitivity reactions with the production of antigen-specific IgE and allergic responses. IL-4 and IL-13 induce clonal expansion of B cells and IgE production. IL-5 recruits and activates eosinophils.
The protective immune response is Th1-type when the infection is caused by intracellular pathogens and Th2-type when it is caused by extracellular organisms (antiparasitic action). The difference in cytokine production between Th1 and Th2 cells underpins the concept of immune deviation.
Insulin resistance
High blood glucose levels are toxic. These levels are regulated by insulin, which activates receptors that allow glucose to enter cells, and by other hormones, one of the most important of which is IGF-1. Low IGF-1 favors diabetes and aggravates cardiovascular diseases.
Insulin response can get worse for several reasons, such as sedentarity lifestyle, obesity..: it is then called insulin resistance (IR).
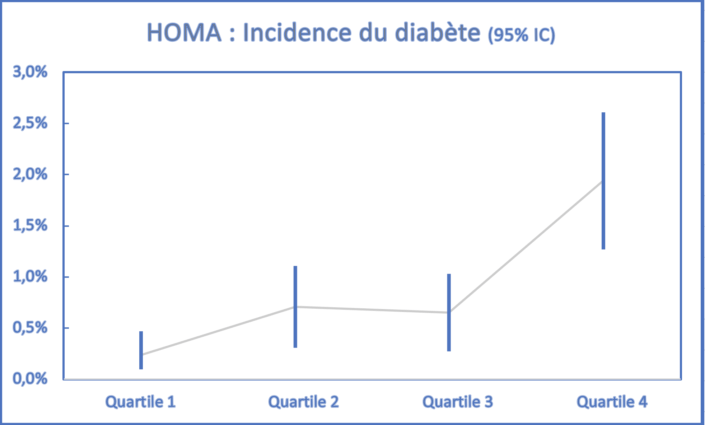
Several pathologies can result from it, including an increased risk of type II diabetes. Advantages of HOMA and Quicki indexes (they complement each other) is that they enable early detection of insulin resistance, which can be corrected through daily exercise and an optimized diet, such as omega-3 fatty acids.
Figure 1:
Incidence of diabetes according to quartiles of HOMA results distribution.
Study on 1680 person-years.
Journal IGF-1 and diabetes: DiabetesCare 33:2257–2259, 2010
Journal IGF-1: BiochimBiophysActa Mol Basis Dis. 2018 May;1864(5 Pt B):1931-1938. doi: 10.1016/j.bbadis.2017.08.029. Epub2017 Aug25. Review.
HOMA and Quicki: Scandinavian Journal of Clinical and Laboratory Investigation, DOI: 10.1080/00365513.2017.1306878
Reference IR and exercice: IntJ BehavNutrPhys Act. 2013 Jan 28;10:10. doi: 10.1186/1479-5868-10-10.
Vitamins
Vitamins are molecules that are not synthesized by the body (except for vitamin D) and are essential. They have various functions in the body. To make it simple, here are some of the most important functions of vitamins.
As for dietary intake, we suggest you go on the Internet using the name of the vitamin + diet.
- Vitamin A: Vitamin A deficiciency may manifest itself through vision issue, lower resistance to infections and/or skin dryness. Chronic poisoning may cause liver disorders.
- Vitamin E: A good antioxidant and a nutrient for the proper functioning of numerous organs, nerves and muscles. A deficiciency may manifest itself through neuromuscular, hematological or immune signs.
- Vitamin C: A good antioxidant. It is needed for the synthesis of collagen and red blood cells, and contributes to the immune system.
- Vitamin B12: It has a hematinic role, helps with the absorption of folic acid (vitamin B9) and helps protect nerve cells. Deficiency in vitamin B12 is a common situation encoutered in geriatrics, from 65 years old, and in diets without meat, milk, cheese, eggs (vegan diet). In case of deficiency, a hyperhomocysteinemia may be observed.
- Vitamin B9 (folates): Folates act as coenzymes in many reactions, including the “de novo” synthesis of purines necessary for DNA synthesis. A folate deficiency leads to anemia. During pregnancy, folate intake is crucial to prevent neural tube defects.
- Vitamin B3 – niacin + nicotinamide – PP: B vitamins help the body to convert food (carbohydrates) in energy (glucose). Niacin is useful for stress-related hormone regulation and improves blood circulation. Symptoms of a slightly deficiency are indigestion, fatigue, vomiting or depression. It may be due to pregnancy or alcoholism.
- Vitamin B1 – Thiamine: It is necessary for the transformation of carbohydrates into energy by the Krebs cycle, and is necessary for the proper functioning of muscles and nervous system. Indeed, it is essential to the transformation of pyruvate produced by glycolysis and toxic for the nervous system.
- Vitamin B2 – Riboflavin: The vitamin B2 plays a key role in the transformation of simple food (carbohydrates, lipids and proteins) into energy. It plays a role in muscle repair metabolism.
- Vitamin B6 – pyridoxine + pyridoxal: It is necessary for the proper cellular functioning, in particular the nervous and skin system.
- Vitamin D (25-OH): 25-OH vitamin D, which includes D2 and D3, represents the body’s vitamin D reserves derived from nutrition and skin production (under the effect of sunlight). Vitamin D acts on more than 200 genes and is particularly important for bone formation, the immune system and brain function.
- Vitamin H – Biotin – (Vitamin B7 or B8): Biotin is a coenzyme which participates to the metabolism of fatty acids, carbohydrates and amino acids as well as the biosynthesis of vitamin B9 and B12. It is useful for skin, hair and nail support.
- Vitamin K1: Vitamin K1 plays an essential role in blood coagulation. It is involved in the maturation of factors in the endogenous pathway (factor IX), the exogenous pathway (factor VII), the common pathway (factors II and X), and proteins C and S, which are coagulation inhibitors.

A discreet presence, a reliable support.
A special need? A doubt about a procedure?
Our team remains available, if you need anything.